Dissociatives
This article is a stub. As such, it may contain incomplete or wrong information. You can help by expanding it. |
Dissociatives (also referred to as dissociative anesthetics) are a class of hallucinogen. Members of this class are characterized by distorted sensory perceptions and feelings of disconnection or detachment from the environment and self. The phenomenology is often described in terms of reducing or blocking signals to the conscious mind from other parts of the central nervous system.[1]
Many dissociatives have general depressant effects and can produce sedation, respiratory depression, analgesia, anesthesia, and ataxia, as well as cognitive and memory impairment and amnesia. Some dissociatives affect the dopamine[2] and/or opioid[3] systems and are capable of inducing euphoria.
Dissociatives can produce a range of subjective effects similar to psychedelics: closed-eye visuals, time distortion, enhanced introspection, conceptual thinking, euphoria, and ego loss.[4][5][6][7]
Mechanism of action
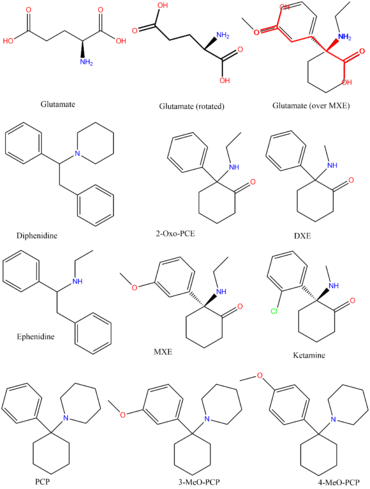
NMDA receptors within the brain exist to allow for the transfer of electrical signals between neurons in the brain and in the spinal column. For electrical signals to pass, the NMDA receptor must be open. To remain open, the neurotransmitters known as glutamate and glycine must bind to the NMDA receptor. An NMDA receptor that has glycine and glutamate bound to it and has an open ion channel is called "activated."
Dissociatives are classed as NMDA receptor antagonists. This means they bind to the receptor, but do not activate it and block other neurotransmitters from doing so. The result is a dose dependent decrease in the passing of electrical signals across the brain and an overall disconnection of neurons. This leads onto states of disconnection between conscious parts of the brain and its sensory organs as well as out-of-body experiences and accompanying hallucinations.
Chemical classes
Arylcyclohexylamines
-
- Ketamine
- Phencyclidine (PCP)
- Eticyclidine (PCE)
- Deschloroketamine (DCK)
- 2-Fluorodeschloroketamine (2-FDCK)
- Methoxetamine (MXE)
- Deoxymethoxetamine (DMXE)
- 3-HO-2'-Oxo-PCE (HXE)
- Methoxpropamine (MXPr)
- Methoxisopropamine (MXiPr)
- O-PCE
- 3-HO-PCP
- 3-Me-PCP
- 3-MeO-PCP
- 4-MeO-PCP
- 3-HO-PCE
- 3-MeO-PCE
- 3-MeO-PCMo
- Methoxyketamine (MXM)
Morphinans
-
- Dextromethorphan (DXM)
- Dextrorphan (DXO)
Others
-
- Ibogaine
- Diethyl Ether
- Huperzine A
- Nitrous oxide
- Xenon
- Galantamine
- Memantine
- Salvinorin A
Subjective effects
Disclaimer: The effects listed below cite the Subjective Effect Index (SEI), an open research literature based on anecdotal user reports and the personal analyses of PsychonautWiki contributors. As a result, they should be viewed with a healthy degree of skepticism.
It is also worth noting that these effects will not necessarily occur in a predictable or reliable manner, although higher doses are more liable to induce the full spectrum of effects. Likewise, adverse effects become increasingly likely with higher doses and may include addiction, severe injury, or death ☠.
Visual effects
-
Suppressions
-
Distortions
-
Geometry
In comparison to other classes of hallucinogen, this effect is significantly less complex and intricate with a limited range of effects. It does not extend beyond level 4 and is variable within most of its variations but is exclusively simplistic in complexity, unstructured in organization, dimly lit in lighting, slow in movement and immersive in depth.
-
Hallucinatory states
- Perspective alterations
- Autonomous entities
- Scenarios and plots
- Settings, sceneries, and landscapes
- Shadow people
External hallucinations
In comparison to other classes of hallucinogen, this effect can occur at heavy dosages, but is extremely infrequent in comparison to the same effect found within deliriants.It can be comprehensively described through its variations as delirious in believability, autonomous in controllability and solid in appearance.
The most common theme for this effect to follow is one of experiencing and talking to friends around oneself when they are not actually present.
Internal hallucinations
In comparison to other classes of hallucinogen, this effect can occur at heavy dosages but is considerably less common than the same effect found within psychedelics and deliriants.It can be comprehensively described through its variations as delirious in believability, fixed in style, equal in new experiences and memory replays in content, autonomous in controllability and solid in appearance.
Disconnective effects
Cognitive effects
-
- Amnesia
- Conceptual thinking
- Cognitive euphoria
- Déjà vu
- Depersonalization
- Derealization
- Dream potentiation
- Increased music appreciation
- Analysis suppression
- Introspection
- Memory suppression
- Personal bias suppression
- Autonomous voice communication
- Thought connectivity
- Thought deceleration
- Thought loops
- Time distortion
- Unity and interconnectedness
Physical effects
Auditory effects
Multisensory effects
See also
External links
Literature
- Morris, H., & Wallach, J. (2014). From PCP to MXE: A comprehensive review of the non-medical use of dissociative drugs. Drug Testing and Analysis, 6(7–8), 614–632. https://doi.org/10.1002/dta.1620
References
- ↑ Tamminga, C. A., Tanimoto, K., Kuo, S., Chase, T. N., Contreras, P. C., Rice, K. C., Jackson, A. E., O’Donohue, T. L. (1987). "PCP-induced alterations in cerebral glucose utilization in rat brain: blockade by metaphit, a PCP-receptor-acylating agent". Synapse (New York, N.Y.). 1 (5): 497–504. doi:10.1002/syn.890010514. ISSN 0887-4476.
- ↑ Giannini, A. J., Eighan, M. S., Loiselle, R. H., Giannini, M. C. (April 1984). "Comparison of haloperidol and chlorpromazine in the treatment of phencyclidine psychosis". Journal of Clinical Pharmacology. 24 (4): 202–204. doi:10.1002/j.1552-4604.1984.tb01831.x. ISSN 0091-2700.
- ↑ Giannini, A. J., Underwood, N. A., Condon, M. (November 2000). "Acute ketamine intoxication treated by haloperidol: a preliminary study". American Journal of Therapeutics. 7 (6): 389–391. doi:10.1097/00045391-200007060-00008. ISSN 1075-2765.
- ↑ Bowdle, Andrew T.; Radant, Allen D.; Cowley, Deborah S.; Kharasch, Evan D.; Strassman, Rick J.; Roy-Byrne, Peter P. (1998-01-01). "Psychedelic Effects of Ketamine in Healthy Volunteers". Anesthesiology. Ovid Technologies (Wolters Kluwer Health). 88 (1): 82–88. doi:10.1097/00000542-199801000-00015. ISSN 0003-3022.
- ↑ Jansen, Karl L.R. (2000). "A Review of the Nonmedical Use of Ketamine: Use, Users and Consequences". Journal of Psychoactive Drugs. Informa UK Limited. 32 (4): 419–433. doi:10.1080/02791072.2000.10400244. ISSN 0279-1072.
- ↑ Kolp, Eli; Friedman, Harris L.; Krupitsky, Evgeny; Jansen, Karl; Sylvester, Mark; Young, M. Scott; Kolp, Anna (2014-07-01). "Ketamine Psychedelic Psychotherapy: Focus on its Pharmacology, Phenomenology, and Clinical Applications". International Journal of Transpersonal Studies. 33 (2): 93–96. doi:10.24972/ijts.2014.33.2.84. ISSN 1321-0122.
- ↑ Reissig, Chad J.; Carter, Lawrence P.; Johnson, Matthew W.; Mintzer, Miriam Z.; Klinedinst, Margaret A.; Griffiths, Roland R. (2012-04-13). "High doses of dextromethorphan, an NMDA antagonist, produce effects similar to classic hallucinogens". Psychopharmacology. Springer Science and Business Media LLC. 223 (1): 1–15. doi:10.1007/s00213-012-2680-6. ISSN 0033-3158.