Derealization
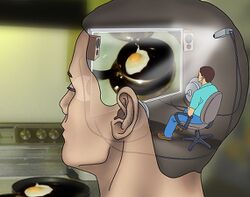
Derealization or derealisation (sometimes abbreviated as DR) is medically recognized as the experience of feeling detached from, and as if one is an outside observer of, one's surroundings.[1][2] This effect is characterized by the individual feeling as if they are in a fog, dream, bubble, or something watched through a screen,[3] like a film or video game.[4] These feelings instill the person with a sensation of alienation and distance from those around them.
Derealization can be distressing to the user, who may become disoriented by the loss of the innate sense that their external environment is genuinely real. The loss of the sense that the external world is real can make it feel inherently artificial and lifeless.[4]
This state of mind is commonly associated with and often coincides with depersonalization. While derealization is a perception of the unreality of the outside world, depersonalization is a subjective experience of unreality in one's sense of self.
Derealization is often accompanied by various perceptual distortions such as visual acuity suppression, visual acuity enhancement, and perspective distortions.[4] Other coinciding effects include auditory distortions and depersonalization.[3][4] This effect is most commonly induced under the influence of moderate dosages of dissociative compounds, such as ketamine, PCP, and DXM. However, it can also occur to a lesser extent during the withdrawal symptoms of stimulants and depressants.
Analysis
In psychiatry, chronic derealization that arises during sobriety is identified as "Depersonalization/Derealization Disorder" and is classified by both the DSM5 and ICD-11 as a single dissociative disorder.[2][4]
Temporary derealization symptoms lasting hours to days are common in the general population. Approximately one-half of all adults have experienced at least one episode of depersonalization/derealization within their lifetime, and the gender ratio for the disorder is 1:1.[4] Chronic derealization is more common within individuals who have experienced a severe trauma or prolonged stress and anxiety. The symptoms of both chronic derealization and depersonalization are common within the general population, with a lifetime prevalence of up to 26-74% and 31–66% at the time of a traumatic event.[5]
This effect is a type of cognitive and perceptual dysregulation.[1] It has been demonstrated that derealization may be caused by a dysfunction within the brains visual processing center (occipital lobe) or the temporal lobe, which is used for processing the meaning of sensory input, language comprehension, and emotion association.[6]
Psychoactive substances
Compounds within our psychoactive substance index which may cause this effect include:
- 2-Fluorodeschloroketamine
- 3-Cl-PCP
- 3-FPM
- 3-HO-PCE
- 3-HO-PCP
- 3-MeO-PCE
- 3-MeO-PCMo
- 3-MeO-PCP
- 4-MeO-PCP
- 6-APB
- Blue Lotus
- Cannabis
- Datura
- Deschloroketamine
- Desoxypipradrol
- Dextromethorphan
- Diphenhydramine
- Diphenidine
- Ephenidine
- Gabapentin
- HXE
- JWH-018
- Ketamine
- MDA
- MDMA
- MXiPr
- Memantine
- Methoxetamine
- Methoxphenidine
- Methylphenidate
- Myristicin
- Nitrous
- O-PCE
- PCE
- PCP
- Pregabalin
- Rolicyclidine
- Selective serotonin reuptake inhibitor
Experience reports
Annectdotal reports which describe this effect with our experience index include:
- Experience: 300mg DXM (Oral) - Brink of the third
- Experience:100-350mg - Phenylpiracetam in daily life
- Experience:3-MEO-PCMo (420mg) - Trip Report
- Experience:300mg DPH + 600mg DXM - An Interesting Combo
- Experience:535mg - My First DXM Trip
- Experience:DXM and Cannabis: 100mg - Unexpected Strong Trip
- Experience:MXE: 37.5 mg - Calm and Cloudy Bliss
- Experience:Nitrous oxide (approx. 50 puffs) - ~50 puffs nitrous oxide
- Experience:Unknown Dose DOC (Insufflated) - Overdosing and Terifying Ego Death
- Experience:~150mg MDA(oral) - a case of mistaken identity
See also
External links
References
- ↑ 1.0 1.1 "Glossary of Technical Terms". Diagnostic and statistical manual of mental disorders (5th ed.): 818–20. 2013. doi:10.1176/appi.books.9780890425596.GlossaryofTechnicalTerms.
- ↑ 2.0 2.1 "Depersonalization-derealization disorder". International statistical classification of diseases and related health problems (11th ed.). 2022. Retrieved 20 May 2022.
- ↑ 3.0 3.1 Espiard, M.-L., Lecardeur, L., Abadie, P., Halbecq, I., Dollfus, S. (August 2005). "Hallucinogen persisting perception disorder after psilocybin consumption: a case study". European Psychiatry. 20 (5–6): 458–460. doi:10.1016/j.eurpsy.2005.04.008. ISSN 0924-9338.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Dissociative Disorders. Diagnostic and statistical manual of mental disorders (5th ed.) (Fifth Edition ed.). American Psychiatric Association. 22 May 2013. doi:10.1176/appi.books.9780890425596.dsm08. ISBN 9780890425558.
- ↑ Hunter, E. C. M., Sierra, M., David, A. S. (1 January 2004). "The epidemiology of depersonalisation and derealisation". Social Psychiatry and Psychiatric Epidemiology. 39 (1): 9–18. doi:10.1007/s00127-004-0701-4. ISSN 1433-9285.
- ↑ Sierra, M., Lopera, F., Lambert, M. V., Phillips, M. L., David, A. S. (1 April 2002). "Separating depersonalisation and derealisation: the relevance of the "lesion method"". Journal of Neurology, Neurosurgery & Psychiatry. 72 (4): 530–532. doi:10.1136/jnnp.72.4.530. ISSN 0022-3050.